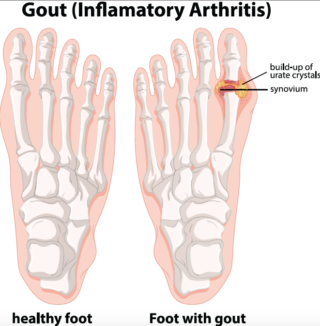
Gout is a common and complex form of arthritis that can affect anyone. It’s characterized by sudden, severe attacks of pain, swelling, redness and tenderness in the joints, often the joint at the base of the big toe.
An attack of gout can occur suddenly, often waking you up in the middle of the night with the sensation that your big toe is on fire. The affected joint is hot, swollen and so tender that even the weight of the sheet on it may seem intolerable.
The pain of Gout is caused by deposits of crystals derived from uric acid. Additional information about gout can be found here at Rheumatology.org.
Gout signs and symptoms almost always occur suddenly, and often at night. Attacks often occur as severe flare-ups typically in the feet and ankles and include:
- Intense joint pain
- Lingering discomfort and selling
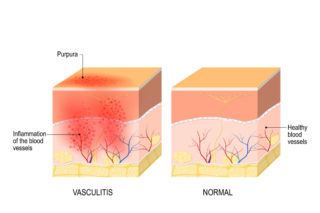
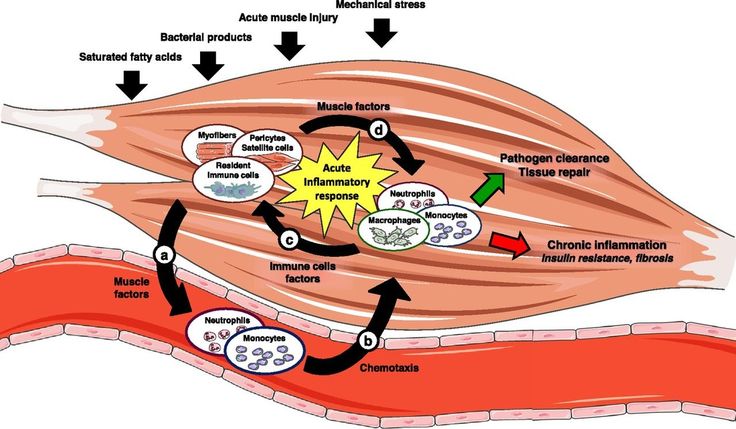
- Inflammation and redness
- Limited range of motion.
Early in the course of this disease, flare-ups occur infrequently, last a week or so, and resolve on their own or with the help of medications that fight inflammation.
Over time, attacks become more frequent, last longer and involve an increasing number of joints. Eventually, if not controlled, gout sufferers may develop persistent joint pain, swelling, deformity and disability. If Gout goes untreated it can lead to worsening pain and joint damage.
During symptom-free periods, dietary guidelines may help protect against future gout attacks:
- Drink plenty of fluids
- Limit or avoid alcohol
- Get your protein from low-fat dairy products
- Limit your intake of meat, fish and poultry
- Maintain a desirable body weight
- Joint fluid test
- Blood test
- X-ray imaging
- Ultrasound
Tests to help diagnose gout include:
- Joint fluid test
- Blood test
- X-ray imaging
- Ultrasound
- Dual energy CT scan
If you experience several gout attacks each year, or if your gout attacks are less frequent but particularly painful, your doctor may recommend medication to reduce your risk of gout-related complications. If you already have evidence of damage from gout on joint X-rays, or you have tophi, chronic kidney disease or kidney stones, medications to lower your body’s level of uric acid may be recommended. Options include:
- Medications that block uric acid production.
- Medication that improves uric acid removal.
AZIV Infusion provides the following biologic injections and infusions in a convenient and comfortable setting for patients seeking treatment for Gout: